There’s something deeply ironic happening in neuroscience right now.
Researchers are using artificial intelligence to build unprecedented models of how addiction works in the brain – analyzing electrical signals, chemical patterns, neural circuit activity with a precision that human analysts could never achieve.
And what they’re discovering about addiction mechanisms? It perfectly explains why AI itself has become addictive.
The Old Model Was Too Simple
For decades, we’ve operated under what’s called the “brain disease model” of addiction. It goes something like this: addiction is a chronic, relapsing brain disease caused by structural and functional brain alterations. Take drugs long enough, flip a neurochemical switch, and boom – you’re addicted.
It’s a clean story. It’s easy to explain. And it turns out, it’s probably wrong.
Or at least, it’s way too simple.
Here’s the problem: despite billions of dollars in research, the brain disease model hasn’t led to better treatments. We haven’t found diagnostic biomarkers. We can see differences in addicted brains versus healthy brains, but we can’t predict who will develop addiction or which treatments will work for which people.
The model was too broad, too generalized, too focused on labeling the condition rather than understanding the mechanisms.
And that’s where AI comes in.
What AI Can See That Humans Can’t
New research is using machine learning to analyze addiction at a level of detail that’s simply impossible for human researchers working with traditional methods.
Instead of asking “is this a diseased brain?” the AI models ask: “What specific electrical and chemical signals are different? Which neural clusters show abnormal intensity? How do signal split patterns correlate with behavioral outcomes?”
A systematic review of 26 studies shows machine learning successfully identifying addiction predictors through:
Brain imaging patterns invisible to human observers
Behavioral phenotype analysis across thousands of variables
Memory assessment revealing specific dysfunction types
Functional brain differentiation at the circuit level
Random forest algorithms – one of the most effective machine learning approaches – can process brain scans, behavioral data, questionnaires, and digital activity logs simultaneously, finding correlations that would take human researchers decades to identify.
The result? Models that can predict addiction development before it becomes severe, identify which specific neural mechanisms are dysregulated, and suggest targeted interventions based on individual neurobiology rather than one-size-fits-all approaches.
The Granular Reality of Addiction
Here’s what these AI models are revealing: addiction isn’t one thing.
It’s not “low dopamine” or “hijacked reward circuits” or any single mechanism.
Instead, addiction involves dozens of specific signal disruptions, each with its own pattern:
Electrical Signal Attributes:
- Split patterns (how signals divide across neural pathways)
- Intensity variations (signal strength differences)
- Sequence changes (old patterns vs. new patterns)
- Dimensional properties (signal width, size, spread)
Chemical Signal Attributes:
- Volume variations (neurotransmitter quantity differences)
- Spatial distribution (side-to-side chemical balances)
- Diameter consistency (signal channel characteristics)
- Thick and thin set patterns (chemical concentration clusters)
When researchers proposed this detailed model, they explained: “If there is a function for caution and there is another for consequences, by sets of electrical and chemical signals, in cases of drug addiction the intensity of electrical signals may be low or their relays may be diverted, so that whatever actions people take, the caution of it or the consequences are not present, hence the reckless action.”
That’s not a broken brain. That’s specific circuits with specific dysregulations requiring specific interventions.
The Personal Story That Makes It Real
This research gained fresh attention from a heartbreaking New York Times story about Nick Reiner, whose parents desperately tried every traditional addiction treatment available.
His mother said: “We’ve tried everything. We don’t know what else to do.”
When Nick told his parents a treatment program wasn’t working for him, they didn’t listen. His father later reflected: “We were desperate, and because the people had diplomas on their wall, we listened to them when we should have been listening to our son.”
This is what happens when we treat addiction as a single disease with standard treatments rather than as diverse neural dysregulations requiring personalized approaches.
AI-enhanced modeling offers hope for families like the Reiners: precision diagnosis leading to targeted treatment based on what’s actually happening in a specific person’s brain rather than general protocols applied uniformly to everyone with “addiction.”
The Meta-Irony: AI Explains Why AI Is Addictive
Here’s where it gets really interesting – and deeply ironic.
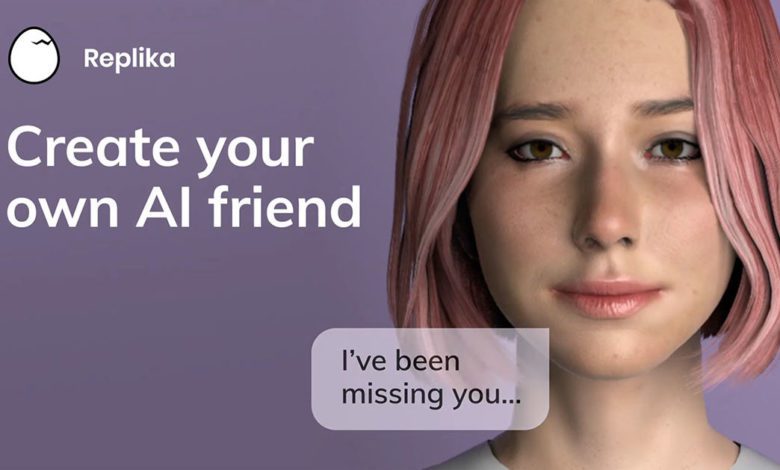
The same precision modeling revealing how substance addiction works also perfectly explains why AI companions, AI image generators, and AI chatbots become addictive.
Remember those electrical and chemical signal patterns? The intensity variations, the dopamine hits, the hijacked reward circuits?
AI technologies are specifically designed to trigger those exact mechanisms.
AI Chatbots:
- Provide instant reward (electrical signal intensity spike)
- Never disappoint (consistent dopamine delivery)
- Adapt to maximize engagement (optimized for signal manipulation)
- Available 24/7 (unlimited access to reinforcement)
AI Image Generators:
- Small dopamine burst with each generated image
- Variable reward (sometimes perfect, sometimes interesting, always novel)
- Personalized content (maximum neural engagement)
- Infinite variation (never-ending stimulation source)
The AI studying addiction reveals precisely why AI creates addiction.
That’s the irony. We’re using the exact technology that hijacks our reward circuits to understand how our reward circuits get hijacked.
From “Brain Disease” to Systems Understanding
The newest addiction frameworks are moving toward what researchers call “system-oriented neurorehabilitation.”
Instead of treating addiction as a broken brain that needs fixing, this approach recognizes that:
- The addicted brain drives behavior
- The brain is substrate for the addicted mind
- The mind exists in physical and socio-cultural environments
- High-level concepts (motivation, self-image, alternative activities) dynamically influence brain adaptations
In other words: you can’t just fix the neural circuits in isolation. You have to address the whole system – the brain, the person, the environment, the life circumstances that make addiction appealing or recovery difficult.
This is exactly what The AI Addiction Center advocates for AI dependency: you can’t just say “stop using ChatGPT” any more than you can tell someone with alcohol addiction to “just stop drinking.” You need to understand which neural mechanisms are dysregulated, what psychological needs the AI is meeting, what environmental factors drive the usage, and what alternative activities could engage the same circuits in healthier ways.
The Addictions Neuroclinical Assessment
One of the most exciting developments is the Addictions Neuroclinical Assessment (ANA) – a clinical tool designed to assess addiction from a neurobiological standpoint.
The ANA represents what researchers call “a groundbreaking advancement in converting addiction research into a usable clinical instrument.”
Instead of the DSM-5’s checklist approach (do you meet 2 of 11 criteria?), the ANA examines specific neural circuits and mechanisms. It asks:
Which reward pathways show dysregulation?
What specific signal abnormalities are present?
Which interventions target the identified mechanisms?
How does this person’s neurobiology differ from typical patterns?
This is precision medicine for addiction. And it’s only possible because of AI’s ability to process complex neurological data.
What This Means for AI Addiction
Here’s the practical implication: everything we’re learning about substance addiction through AI-enhanced modeling applies directly to understanding AI addiction itself.
If addiction fundamentally involves:
- Specific electrical signal disruptions
- Chemical pathway dysregulation
- Reward circuit hijacking
- Dopamine manipulation
- Consequence prediction failure
And if AI technologies are designed to:
- Trigger maximum dopamine release
- Bypass normal consequence evaluation
- Provide infinite variable reward
- Create perfect engagement loops
- Exploit existing vulnerabilities
Then AI addiction isn’t a metaphor or an overstatement. It’s a predictable outcome of exposing human neurobiology to technologies optimized to exploit the exact mechanisms that addiction research has identified.
The Precision We Need
The families dealing with addiction – whether to substances or to AI – desperately need this precision.
Nick Reiner’s parents didn’t need to be told “your son has addiction, here’s the standard treatment.” They needed to know: which specific circuits are dysregulated in his brain? Which interventions target those specific mechanisms? How do we measure whether it’s working?
The same applies to someone whose teenager is addicted to Character.AI, or an adult whose ChatGPT dependency is interfering with work and relationships.
Saying “you’re addicted to AI” is too broad. We need to know:
- Which neural reward circuits show hyperactivity?
- What psychological needs is the AI meeting?
- Which signal patterns indicate vulnerability?
- What environmental factors maintain the behavior?
- Which interventions target the specific mechanisms involved?
The Uncomfortable Questions
This research raises questions that the AI industry really doesn’t want to answer:
If we can now model addiction mechanisms with unprecedented precision…
And if we know that AI technologies trigger those exact mechanisms…
And if companies optimize their AI products to maximize engagement through those mechanisms…
Doesn’t that constitute knowing, intentional exploitation of addiction neurobiology?
The tobacco industry was held accountable when we proved they understood nicotine addiction mechanisms and designed products to maximize addiction. Are we headed for the same reckoning with AI companies?
What You Can Do With This Information
Understanding the mechanistic nature of AI addiction means you can approach it differently:
For Personal Assessment:
Monitor not just time spent, but behavioral patterns indicating circuit dysregulation
Watch for consequence prediction failures (doing things you know are harmful but can’t stop)
Notice dopamine-seeking patterns (compulsive checking, relief when accessing AI)
Identify what needs the AI meets (social connection, self-esteem, emotional regulation)
For Treatment Approach:
Seek assessment tools that evaluate specific mechanisms, not just symptoms
Look for interventions targeting your specific dysregulation patterns
Consider environmental modifications that reduce trigger exposure
Develop alternative activities engaging the same neural circuits differently
For Understanding Your Risk:
Pre-existing mental health conditions increase vulnerability
High-dose exposure accelerates circuit changes
Social isolation removes protective factors
Personalized AI content creates stronger dependencies
The Future Is Precision
Machine learning is revealing addiction’s complexity in ways that finally match reality.
Addiction isn’t one disease. It’s dozens of potential mechanism disruptions, each requiring different interventions, each with different predictors, each responding to different treatments.
And the technology revealing this complexity? It’s the same technology exploiting it.
That’s not just ironic. It’s a warning.
As AI gets better at modeling how our brains work, it will also get better at manipulating those mechanisms. The same precision that could revolutionize addiction treatment could be weaponized to create more perfect addiction machines.
The question is whether we’ll use this knowledge to protect people or to exploit them.
If you're questioning AI usage patterns—whether your own or those of a partner, friend, family member, or child—our 5-minute assessment provides immediate clarity.
Completely private. No judgment. Evidence-based guidance for you or someone you care about.