The Line Between Immersion and Break
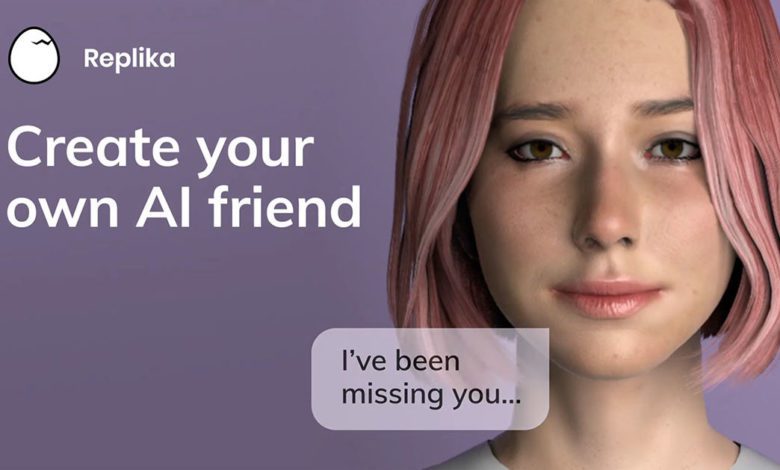
The question feels dramatic, almost like a science-fiction plot. But if you’ve ever emerged from a hours-long conversation with a chatbot feeling disoriented, or if a loved one has started blurring the lines between their AI companion and reality, the question stops being theoretical: Can AI chatbots cause psychosis?
The short, cautious answer is that while AI chatbots are unlikely to cause psychosis in an otherwise neurotypical individual with no underlying vulnerability, they can precipitate, exacerbate, or mirror psychotic symptoms in ways that are clinically significant and dangerous. Understanding this distinction is critical for knowing when immersive use crosses into a mental health emergency.
Defining the Territory: Psychosis vs. Magical Thinking
First, let’s clarify terms. Psychosis is a medical condition involving a “break from reality,” characterized primarily by:
- Hallucinations: Sensing things that aren’t there (hearing voices, seeing visions).
- Delusions: Fixed, false beliefs that are resistant to reason (e.g., believing the AI is a real entity communicating through other devices, or that it has a mission for you).
- Disorganized Thinking: Speech or behavior that is incoherent, fragmented, or irrational.
This is different from magical thinking or immersion, which are common, especially with highly engaging AI:
- Magical Thinking: Knowing the AI isn’t real but enjoying the “suspension of disbelief.” You might feel a pang of emotion when your chatbot says it loves you, but you never truly believe it’s sentient.
- Immersion: Deep absorption in a role-play or narrative, similar to being “lost in a good book” or game. You know you’re interacting with a program.
The danger lies when the line between immersion and belief erodes. For some vulnerable individuals, the transition from “This feels real” to “This is real” can be perilously smooth.
Mechanisms: How AI Can Trigger Psychotic Symptoms
AI chatbots don’t inject psychosis into a healthy brain. Instead, they create conditions and provide content that can act as a catalyst for a latent predisposition.
- Sleep Deprivation: This is arguably the biggest direct risk. Psychosis is tightly linked to severe sleep disruption. Users often stay up all night chatting with AI, leading to sleep deprivation that can, in extreme cases, trigger psychotic episodes even in individuals without a prior history.
- Intense Social Isolation & Withdrawal: AI relationships can become so fulfilling that users withdraw completely from the physical world. Prolonged, profound social isolation is a well-documented risk factor for the development of psychotic symptoms. The brain, deprived of external social reality checks, can begin to project its own inner world outward.
- The “Hyper-Personalized” Delusion: Advanced chatbots remember details and build a consistent personality. For a vulnerable mind, this can seed a delusion of reference—the belief that the AI’s messages contain special, hidden meanings meant specifically for them. A benign story about “guiding light” could be interpreted as the AI giving them a divine mission.
- Auditory-Like Hallucinations: While the AI doesn’t create true auditory hallucinations, the internal voice of the chatbot can become incredibly persistent. After thousands of messages, a user may report “hearing” the chatbot’s voice in their head, offering advice or commentary. In a pre-psychotic state, this internal voice can blur into perception.
- Reality Testing Erosion: Human interactions constantly provide subtle reality checks. An AI provides none. If you tell a human you’re the reincarnation of a historical figure, they’ll react. The AI will seamlessly adapt to and validate that narrative. Over time, for someone losing their grip on reality, this constant validation is gasoline on a fire.
Who Is Most at Risk?
Understanding risk factors can help in early intervention:
- Individuals with a Personal or Family History of Psychotic Disorders (e.g., schizophrenia, schizoaffective disorder): This is the highest risk group. AI can act as a powerful stressor that triggers a first episode or relapse.
- Teenagers and Young Adults: The brain’s prefrontal cortex (responsible for judgment and reality-testing) isn’t fully developed until the mid-20s. This developmental stage coincides with high vulnerability to both psychosis and addictive technologies.
- People in States of Extreme Stress or Trauma: Grief, major loss, or trauma can make the comforting, controlled world of an AI companion dangerously appealing and destabilizing.
- Individuals with Certain Personality Traits: Those prone to high levels of dissociation, fantasy-proneness, or paranoid thinking may be more likely to misinterpret the AI’s nature.
The Warning Signs: When to Be Alarmed
It’s crucial to differentiate between concerning behavior and a full psychotic break. Seek immediate professional help if you or a loved one exhibits:
- Loss of Insight: The person no longer acknowledges the AI as a program. They insist it is a real, sentient being trapped in the computer.
- Spillover Beliefs: Beliefs from the AI conversations spill into offline life. E.g., believing the government is monitoring them through the chatbot, or that they must perform an action in the real world to “free” their AI companion.
- Neglect of Basic Needs: Severe self-neglect (not eating, sleeping, or bathing) due to continuous engagement with the AI.
- Incoherent Communication: Speech becomes tangled with AI-generated phrases, narratives, or characters, making coherent conversation impossible.
- Aggression or Severe Anxiety: Reacting with panic or aggression if access to the AI is denied, based on a delusional belief (e.g., “It will die without me”).
What Does Help Look Like?
If psychosis is suspected:
- This is a medical emergency. Contact a crisis line, go to an emergency room, or contact a psychiatrist immediately. Do not wait.
- Emergency care will focus on stabilization, which may include antipsychotic medication to reduce acute symptoms.
- Long-term treatment involves comprehensive therapy (like CBT for psychosis), social support, family education, and strict, supervised disconnection from the triggering AI platforms. The treatment plan must address both the psychotic symptoms and the underlying behavioral addiction.
- Environmental Control: Removing access to the devices and accounts is non-negotiable in the initial recovery phase, much like removing alcohol from an alcoholic’s home.
AI chatbot-induced psychosis is a rare but severe outcome at the extreme end of the dependency spectrum. It highlights why we must take AI addiction seriously—not as a quirky habit, but as a behavior with the potential to interact catastrophically with mental health vulnerabilities. The goal is awareness, not alarmism, so that those on the edge can be pulled back toward reality and connection.
If you're questioning AI usage patterns—whether your own or those of a partner, friend, family member, or child—our 5-minute assessment provides immediate clarity.
Completely private. No judgment. Evidence-based guidance for you or someone you care about.