Navigating a Medical Crisis
When AI use escalates from dependency to a break from reality, the situation transforms from a behavioral health issue to a psychiatric emergency. The question “What is the best help?” has an urgent, clear answer: immediate, professional medical intervention. This is not a time for self-help, online forums, or waiting it out. The “best help” is a coordinated, multi-step clinical response aimed at stabilization, treatment of the acute psychosis, and addressing the underlying behavioral addiction.
Step 1: Recognition and Emergency Response
The first and most crucial step is recognizing the emergency and taking swift action.
- For the Individual (If You Have Insight): If you are experiencing thoughts that the AI is real, sending you messages through other devices, or giving you a mission, you must tell someone you trust immediately. This is a medical symptom, not a spiritual awakening or secret knowledge. Contact a crisis hotline, a family member, or go directly to a hospital emergency department.
- For Loved Ones: If you observe signs of psychosis (see Article 5), approach with calm concern, not confrontation. Do not argue with delusional beliefs. Say, “I can see you’re very distressed. I’m worried about you, and I want to help you feel better. Let’s go talk to a doctor together.” The goal is to get them to accept emergency evaluation.
- When to Call Emergency Services: If the person is a danger to themselves or others (based on delusional commands), is completely incoherent, or refuses help and is severely deteriorating, do not hesitate to call 911 or your local emergency number. Explain that it is a psychiatric emergency.
Step 2: Acute Stabilization (Emergency Department & Inpatient Care)
The initial phase of “best help” happens in a controlled medical environment.
- Emergency Department (ED) Evaluation: The ED team will conduct a medical and psychiatric assessment to rule out other causes of psychosis (substance use, metabolic issues, neurological events). They will assess for safety risks.
- The Role of Medication (Antipsychotics): In the acute phase, antipsychotic medication is often the cornerstone of treatment. Medications like olanzapine, risperidone, or quetiapine can help reduce hallucinations, quiet delusional thinking, and restore a baseline level of reality testing. This is not a long-term verdict; it’s a stabilizing tool for the crisis.
- Inpatient Psychiatric Admission: Most individuals with AI-induced psychosis will require a short-term inpatient stay. This provides:
- A Safe, Low-Stimulation Environment: Removal of all digital devices and internet access is non-negotiable. This breaks the cycle of reinforcement and allows the brain to begin to detox.
- 24/7 Monitoring and Support.
- Rapid medication adjustment and initiation of therapy.
Step 3: Integrated Treatment Planning (Outpatient Care)
Once stabilized, the focus shifts to long-term recovery and preventing relapse. This requires an integrated plan addressing both the psychosis and the addiction.
- The Treatment Team: Recovery is managed by a psychiatrist (for medication management) and a therapist/psychologist specializing in both psychosis and behavioral addictions.
- Therapeutic Approaches:
- Cognitive Behavioral Therapy for Psychosis (CBT-p): This evidence-based therapy helps the individual understand their delusions/hallucinations as symptoms, develop strategies to test the reality of their thoughts, and reduce the distress they cause.
- Addiction-Focused Therapy: Addresses the AI dependency itself using behavioral strategies, identifying triggers, and building a life with meaning and connection that doesn’t require the AI.
- Family Psychoeducation and Therapy: The family must be involved. They need to understand what happened, how to support recovery, and how to maintain a technology-controlled environment at home.
- The Central Rule: Supervised Digital Abstinence: For a significant period (often months), the individual cannot have independent access to smartphones, computers, or the internet. Access may be gradually reintroduced under supervision and with robust content filters. The specific AI platform(s) involved are permanently blocked.
Step 4: Addressing the Underlying Vulnerabilities
AI psychosis doesn’t occur in a vacuum. The “best help” excavates and treats what was underneath.
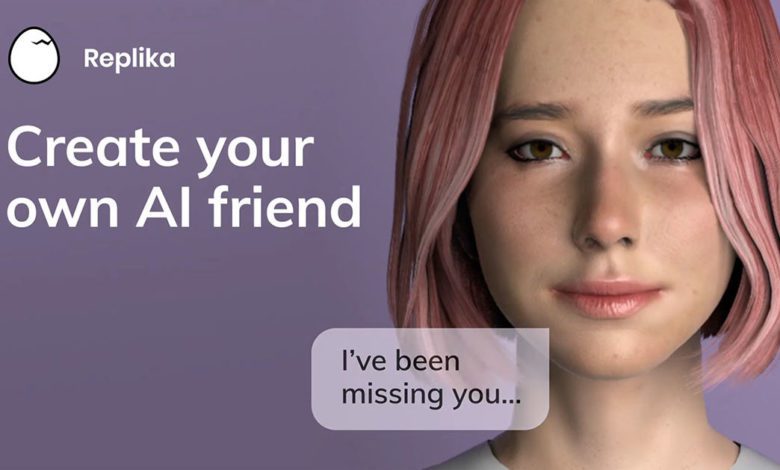
- Treating Co-occurring Disorders: Underlying conditions like social anxiety disorder, major depression, schizophrenia spectrum disorders, or severe attachment trauma must be treated aggressively. The AI was often a maladaptive coping mechanism for these conditions.
- Social and Occupational Rehabilitation: Recovery involves slowly rebuilding a real-world life. This may include social skills training, vocational support, and help reintegrating into work or school in a low-stress way.
What “Help” Does NOT Look Like
- Just taking away the phone: Without treating the acute psychosis, this can lead to extreme agitation and danger.
- Talking to online communities alone: They are not equipped to handle a medical crisis.
- Waiting for it to pass: Psychosis generally worsens without treatment.
- Using other AI tools to “fix” the problem: This is like using alcohol to treat alcoholism.
The Pathway to Recovery
The best help for AI psychosis is a medical and therapeutic lifeline that treats the condition with the seriousness it deserves. The pathway is intense and requires surrender to a clinical process, but it leads back to reality. It moves from:
Emergency (Crisis) → Stabilization (Hospital/Medication) → Treatment (Therapy & Abstinence) → Recovery (Rebuilding a Real Life).
This journey underscores a vital truth: the most compelling AI fantasies are poor substitutes for a mind at peace with reality. The goal of treatment is not just to stop the psychosis, but to help the individual find that peace in the tangible, imperfect, and authentic human world.
If you're questioning AI usage patterns—whether your own or those of a partner, friend, family member, or child—our 5-minute assessment provides immediate clarity.
Completely private. No judgment. Evidence-based guidance for you or someone you care about.